
By the end of this USMLE Step 1 lesson, you will be able to answer the following questions:
- Use mechanism of digoxin to explain effect on contractility.
- Effect of hypokalemia on digoxin effects? Why?
- What histologic changes would you see visually in transient ischemia? Why?
- What is the clinical presentation of someone with hypercalcemia? Why does this make sense?
- What is the clinical presentation of someone with hypocalcemia? Why does this make sense?
- Trousseau’s sign: use the underlying membrane physiology to try and explain why this occurs
Since the USMLE Step 1 is a test of your ability to apply and connect your knowledge, being able to connect such disparate things as reversible cell damage and digoxin effects will be critical to reaching your peak potential. This is the exact strategy I used to score 270 on the USMLE Step 1.
NOTE: Many of these concepts I discuss here build on a previous lesson, which you may want to reference.
Ready for the recall-type USMLE Step 1 questions?
What sets the normal Na/K gradient across the cell membrane?
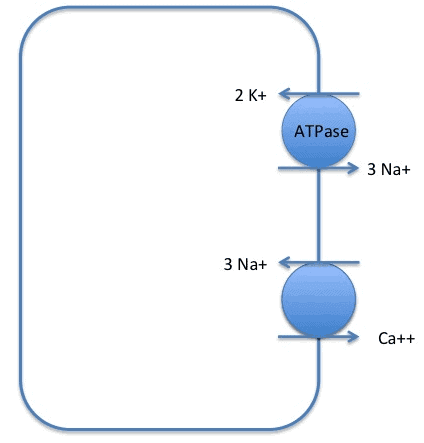
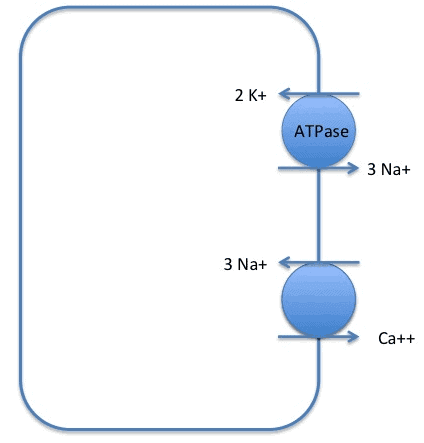
So what does the Na/K ATPase (pump) actually do?
Normally, Na+ would NOT want to move outside the cell, because the outside is POSITIVE relative to the inside, and the Na+ concentration is much higher outside. Thus, we need the energy derived from ATP hydrolysis to drive these ions against their respective gradients.
How many ions of each does it move, and in what direction?
But doesn’t Na+ normally want to move INSIDE the cell?
This is what makes the Na/K ATPase special – it moves Na+ and K+ against their respective concentration gradients, which requires the use of ATP.
What would the membrane potential be if I were to block the Na+/K+ ATPase (more or less negative)?
Recall that the majority of the resting membrane potential is determined by the K+ gradient. In other words, if the K+ gradient ↓ → membrane potential LESS negative
Membrane potential will be more positive (less negative)
What effects would hyperkalemia have on membrane potential?
In other words, since the resting membrane potential is determined largely by K+ conductance (i.e. at rest, there are more K+ channels open than any other ion channels), K+ concentration gradient ↓ → resting membrane potential less negative
Clinically, what ion can you give to someone with hyperkalemia? How is this thought to help?
Ca++ is thought to (and is shown experimentally*) to raise the threshold for depolarization, albeit transiently. Thus, when hyperkalemia ↑ membrane potential, moving it closer to the action potential threshold, you give Ca++ to ↑ the action potential threshold.
What is the mechanism by which Ca++ is pumped out of the cell? What drives this process?
Here, again, Ca++ is moving AGAINST its chemical gradient (recall: there is more Ca++ outside the cell than inside). Thus, the energy provided by Na+ moving DOWN its concentration gradient allows for the transport of Ca++ out.
This is analogous to how the energy from ATP was used to pump Na+ and K+ against their respective concentration gradients.
Digoxin – blocks what protein? At which site?
Binds to the site for K+ binding (i.e. K+ and digoxin compete for the same binding site).
Wait!
I strongly recommend that you attempt to answer the final questions by yourself first, before looking at the answers. Remember, the USMLE Step 1 exam will test your ability to make connections on the spot. The more practice you have, the higher your score! Then, when you think you might know the answer (or are completely stumped), look at the answers below!
Ready to apply your USMLE Step 1 knowledge like a boss?
Use mechanism of digoxin to explain effect on contractility.
Effect of hypokalemia on digoxin effects? Why?
Recall that K+ and digoxin compete for the same binding site (this is competitive inhibition). Thus, if there is less K+ → digoxin will bind more strongly → potentiation of digoxin effects
In other words, BEWARE DIGOXIN TOXICITY IN HYPOKALEMIA
What histologic changes would you see visually in transient ischemia? Why?
What is the clinical presentation of someone with hypercalcemia? Why does this make sense?
We can make sense of this by thinking that Ca++ is increasing the depolarization threshold generally, throughout their body. Thus, they will feel slow (fatigability, lethargy), and be weak (areflexia/weakness) that may even lead to coma.
What is the clinical presentation of someone with hypocalcemia? Why does this make sense?
Take a minute to think about this.
These signs of neuromuscular hyperexcitability include:
Chvostek’s sign: Tapping of facial nerve → contraction of facial muscles (classic sign you should know for USMLE Step 1)
Trousseau’s sign: Occlusion of brachial artery with BP cuff → carpal spasm (another USMLE Step 1 classic)
Hyperactive deep tendon reflexes (more of a Step 2 question, although useful in the grand scheme)
Trousseau's sign: use the underlying membrane physiology to try and explain why this occurs
Since in hypocalcemia, cells are already closer to depolarization, depolarizing the membrane w/ transient ischemia presumably → action potential → muscle contraction.
What should you do next?
- Turn the narrative, “Pathogenesis to Presentation” questions into Anki cards by copy/pasting the question/answer into the “Front” and “Back” fields in Anki. Do the same for the fundamental facts that you were unfamiliar with, to maximize your chances of USMLE Step 1 success! Remember: the USMLE is a test of understanding, so the better you can understand these questions, the better your score!
- Add reverse cards when appropriate to your Anki cards
- Re-word the questions/explanations as desired, and BOLD the important text to make it easier to review in the future
- Learn something new? Something unclear? Comment below!
- If you liked this post, please consider sharing it on Facebook/Twitter! I judge the utility of these posts by the number of comments / shares they receive, so if you’d like more, or would like a particular topic addressed, please let us know!
**Out of curiosity, I looked up to see what literature there was on serum Ca++ levels and membrane excitability. If you’re interested in learning more, there’s a paper on the topic…from 1968(!!!). Awesome!







K+ out of cells should lead to hyper polarization. If I stated otherwise, that is likely a mistake. Can you tell me where this was?
Hi Alec,
I really love this breakdown – definitely helps me understand some of the basic principles!
I have an issue with the potassium channels increasing to increase K+ out which causes depolarization, however. Specifically, I have an issue with it because adenosine causes K to leave which hyperpolarizes the cell – this directly conflicts with your etiology detailed here stating that more K out causes depolarization of the cell membrane. Any explanation for that?
K+ out of cells should lead to hyper polarization. If I stated otherwise, that is likely a mistake. Can you tell me where in the article this was?
So I’m almost there– I’m revisting cellular physio to connect all these points– can you clean this up/clarify for me:
Hyperkalemia (↑ extracell K+) bc resting membrane potential is determined by potassium — although it raises the membrane potential, this sustained depolarization actually causes the slow responding Na+ inactivation gates to remain closed– making it unlikely/impossible for AP to occur in SKELETAL & non-nodal cardiac muscle (correct?) — causing weakness
BUT in nodal cardiac muscle — bc it doesn’t depend on voltage Na+ inactivation/activation gate mechanism, rather only Ca++ conductance– by raising the membrane potential & perhaps passing the depolarization threshold potential w/ hyperkalemia you are MORE likely to get arrhythmia
vs
Hypercalcemia (↑ extracell Ca++) bc has little influence on the membrane potential just raises the depolarization threshold potential (I’m guessing bc there is no conductance Ca++ just a bigger concentration gradient difference) you are LESS likely to have AP in SKELETAL & non-nodal cardiac muscle (same as hyperkalemia)– causing weakness too
BUT in nodal cardiac muscle– bc resting membrane potential is still dependent on K+– you won’t get arrhythmias with hypercalcemia bc you are just raising the depolarization threshold potential making it still less likely for AP to occur
So giving calcium is just to prevent the most dangerous part of hyperkalemia in its effects on the heart? Bc otherwise, you would want to reduce potassium levels to get the resting membrane potential back to normal for the effects on skeletal muscle and non-nodal cardiac tissue.
Thank you! Hope you can help clear this up.
Hi Wisdom Seeker. Wow, lots to address here. First, my understanding is that you want to give Ca++ NOT to control nodal tissue, per se, but because the arrhythmias that will kill you are the ones that start in the ventricle (V-Fib, V-Tach). In other words, you want to decrease the risk of ventricular arrhythmias, and Ca++ can reduce the excitability of ventricular myocytes. You are correct that hyperkalemia can cause weakness, but the main reason you want to treat K+ is because it can be fatal (I had a close family member who passed away recently, presumably because of an arrhythmia, so this is very real, and quite deadly). Thanks again for the feedback – I look forward to hearing from you on other/future articles!
Thank you, but I am confused by the explanation:
1. “Ca++ is thought to raise the threshold for depolarization” – Make it harder for depolarization?
2. “hyperkalemia ↑ membrane potential” – Make it easier for depolarization?
3. “give Ca++ to ↑ the action potential threshold” – Make it harder for depolarization?
Hi FemmeFatale,
Thank you so much for your feedback, and for your great questions. You are correct – hyperkalemia would raise the membrane potential, moving it closer to the depolarization threshold. Thus, hyperkalemia would make it EASIER to set off an action potential. Calcium has the ability to raise the depolarization threshold, thus making it harder to depolarize.
Simply put, hyperkalemia makes it easier to set off an action potential, so we give calcium to people to make it harder to get an action potential again, since ventricular arrhythmias are very dangerous.
Hope this helps!
Alec
Thank you Alec, I’ve been studying Cardio phys + pharm recently, and have been wondering how to best incorporate the 2 in Anki- these are great examples 🙂 many thanks!
Thanks for the positive feedback!! Glad it helped!!!