
By the end of this USMLE Step 1 lesson, you will be able to answer the following questions:
- Erythroblastosis fetalis – associated with ABO incompatibility vs. Rh incompatibility? Why does this make sense?
- How prevent Hemolytic Disease of the Newborn (HDN)/erythroblastosis fetalis in second child in Rh-negative female? Why?
- What are the major benefits of a conjugate vaccine? Why?
- If a patient has A+ RBCs, what antibodies would they produce? Why?
By answering these questions, you will have reviewed these topics (among others): T-cell dependent/independent B-cell activation, conjugate vaccines, ABO/Rh incompatibility.
Ready?
What is the function of B-cells?
What generally do helper T-cells (CD4+) do?
What kinds of macromolecule(s) can you generally activate T-cells against? Why does this make sense?
MHC molecules exhibit protein
What kinds of macromolecule(s) can you generally activate B-cells against?
What is isotype switching? What is required?
Helper T-cells MUST be activated, and then co-activate B-cells in order to isotype switch
If I activate a B-cell against a carbohydrate, what antibody isotypes can I produce? Why does this make sense?
For isotype switching, you would need protein antigens (presented via MHC) which would allow for activation of CD4+ T cells
If I activate a B-cell against a carbohydrate, can I produce IgG?
Recall, also, that T-cells MUST be activated against protein, and T-cells are necessary to induce isotype switching in B-cells from IgM → IgG, etc.
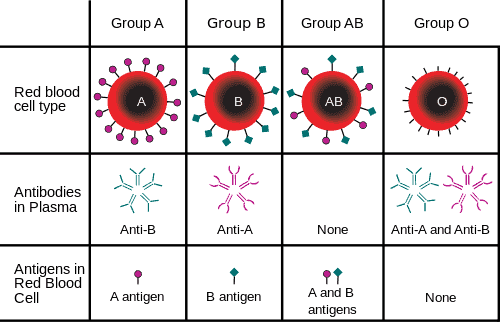
What RBC antigens are regularly tested for in pregnancy?
Why are they such a concern?
If I had antigen A on my RBCs, but no Rh, what would you call me?
What are A or B antigens made of (part of the ABO antigen system) on the RBC?
What kinds of antibodies can you make against sugars? Why?
In order to have isotype switching
What is the Rh antigen made out of on the RBC?
What kinds of antibodies can you make against Rh?
Which antibodies can cross the placenta?
What is passive immunization vs. active immunization?
Vs.
Induce immunity IN patient by giving some sort of ANTIGEN
Erythroblastosis fetalis – what is it?
Basically hemolytic disease of the newborn (antibodies causing hemolysis), but while in utero (technically not hemolytic disease of the newborn, since the baby hasn’t been born yet)
What is more concerning – Rh-negative mother w/ Rh-positive fetus, or an Rh-positive mother w/ Rh-negative fetus? Why?
The fetus has an immature immune system, so would not pass antibodies to the mother
Recall that babies rely on maternal antibodies FOR THE FIRST 6 MONTHS OF LIFE. Thus, if they are B-cell deficient (i.e. btk deficiency) immunodeficient, IT WILL OFTEN PRESENT AROUND 6 MONTHS OF AGE (this is a key Step 1 fact)
When is the mother most likely to become sensitized (produce antibodies against) Rh antigen? Why does this make sense?
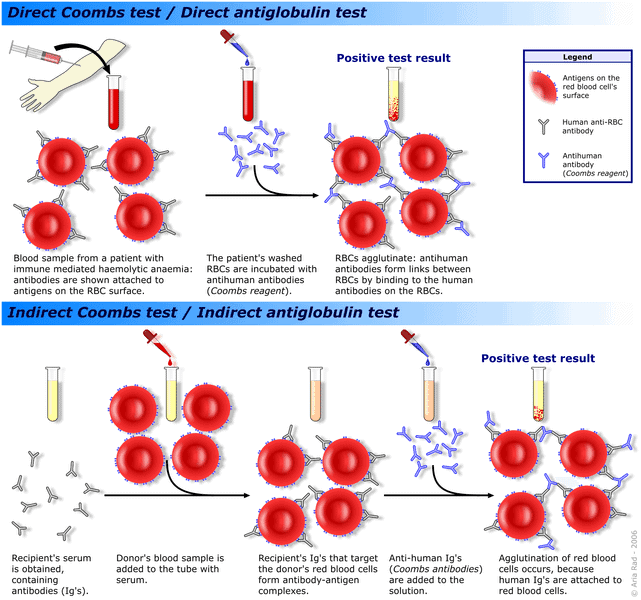
Let’s say you have antibody-coated RBCs in a test tube. If I added an antibody that will bind to antibodies, what would you see happen?
Direct vs. indirect Coombs tests – what is the basis? What are you actually testing for?
Let’s switch gears for a second, and tie in what appears to be completely unrelated (at least on the surface).
Let's go!
What is a bacterial capsule made out of? What bacterium is the exception, and what is its capsule made out of?
Bacillus anthracus – capsule made out of amino acid (glutamate)
What is the antigen used in vaccines against encapsulated organisms?
What is the problem with using ONLY a capsular antigen in a vaccine?
What is a conjugate vaccine?
Wait!
I strongly recommend that you attempt to answer the final questions by yourself first, before looking at the answers. Remember, the USMLE Step 1 exam will test your ability to make connections on the spot. The more practice you have, the higher your score! Then, when you think you might know the answer (or are completely stumped), look at the answers below!
Ready to apply your knowledge like they will ask you for the USMLE Step 1?
Erythroblastosis fetalis - associated with ABO incompatibility vs. Rh incompatibility? Why does this make sense?
Recall that you can make IgG against protein antigens, and since Rh is a protein antigen, you can make IgG, which can cross the placenta. ABO is a carbohydrate antigen, so you CANNOT make IgG against it, since T-cells cannot be activated against it to cause isotype switching in the B-cell.
How prevent HDN/erythroblastosis fetalis in second child in Rh-negative female? Why?
Rho-Gam – anti-Rh antibodies that you inject into the mother, which eliminate the Rh antigen from the mother’s blood stream BEFORE she can develop her own antibodies against it.
What are the major benefits of a conjugate vaccine? Why?
If a patient has A+ RBCs, what antibodies would they produce? Why?
What should you do next?
- Turn the narrative, “Pathogenesis to Presentation” questions into Anki cards by copy/pasting the question/answer into the “Front” and “Back” fields in Anki. Do the same for the fundamental facts that you were unfamiliar with, to maximize your chances of USMLE Step 1 success! Remember: the USMLE is a test of understanding, so the better you can understand these questions, the better your score!
- Add reverse cards when appropriate to your Anki cards
- Re-word the questions/explanations as desired, and BOLD the important text to make it easier to review in the future
- Learn something new? Something unclear? Comment below!
- If you liked this post, please consider sharing it on Facebook/Twitter! I judge the utility of these posts by the number of comments / shares they receive, so if you’d like more, or would like a particular topic addressed, please let us know!
Photos from InvictaHOG and A. Rad







Hi ,
Have you been thinking about a better approach to manage your billing workflow?
Our system is built to handle billing efficiently and reduce headaches from coding and delays.
Our clients often see more streamlined reimbursements and fewer headaches.
Open to seeing how we compare?
Regards,
Dr. Josefina McEwan
Healthcare Solutions Contact
USA Medical Billing LLC
If you’d prefer not to hear from us again, just reply with REMOVE.
This was very helpful and a great refresher! The only commentary I would add is for the question that mentions what antibody isotopes can be produced when triggered by a carbohydrate, followed by why this makes sense. The explanation never states “why” this makes sense. There is also one drop-down arrow that is blank (no question or answer).
Should be fixed now – thanks so much!