After reading this USMLE Step 1 article, you will be able to answer the following questions:
- What ion is primarily responsible for conduction through the AV node? Why?
- What major antiarrhythmic classes are used for rate control in atrial fibrillation? Why does this make sense?
- What is the mechanism of ventricular tachycardia in a-fib? Why would a β-blocker or Ca++ channel blocker help?
- What is more dangerous – atrial fibrillation or ventricular fibrillation? Why does this make sense?
- What would be the EKG findings in WPW? Why does this make sense?
- β blockers primarily affect which major EKG interval? Why?
Ready for the recall-type USMLE Step 1 questions?
What is the order of normal conduction in a healthy heart (i.e., it begins in the SA node, then goes to...).
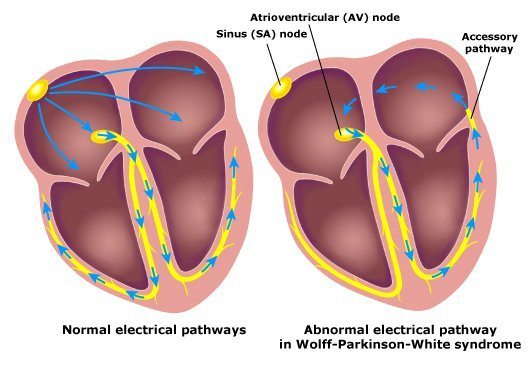
What is the defect in Wolff Parkinson White (WPW) syndrome?
What is the relative speeds of conduction through the following tissue: atrium, ventricle, AV node, His Purkinje
2.2 m/s (Purkinje)
1.1 m/s (atria)
0.3 m/s (ventricles)
0.03 m/s (AV node)
Note that there is a HUGE difference in conduction speed between Purkinje fibers and ventricles/AV node.
What does the P wave represent on an EKG?
What does the QRS complex represent?
What does the T wave represent?
What is the basis for the QRS being wide vs. narrow? Why?
In other words, if depolarization moves through the fast His Purkinje system (by first moving through the AV node), it will be narrow-complex.
Instead, if you have conduction between ventricular myocytes (i.e. NOT through the His Purkinje system), it will be wide-complex.
In WPW, would the QRS be wide or narrow? Why?
There are two sources of excitation of the ventricles in WPW. One source is the normal source: AV node → His Purkinje → ventricular myocytes. However, the other source actually involves ventricular myocytes in the path of the accessory pathway being excited prior to getting by the His Purkinje system, the so-called “pre-excitation.”
How many depolarizations of the atrium are there per heart beat in a healthy patient?
In atrial fibrillation, how many many depolarizations of the atrium are there per heart beat?
How can we make sense of the number of atrial depolarizations on the EKG? Is the entire atrium depolarizing every time, or just part of it?
In other words, one small fragment of the atrium is depolarizing, while another is repolarizing, while a third has already depolarized, and a fourth is…, etc.
There is not a single wave of depolarization moving from the SA → AV node
Let’s make an analogy:
Using this analogy, the single stream of drops would be like the SA nodal depolarization, while the rippling would be like the wave of depolarization that moves through the atrium.
Atrial fibrillation is like having a rainstorm, whereby LOTS of drops are falling all over the pond, causing mini ripples throughout the pond, but NOT a single ripple that will move through the entire pond.
What is the mechanism of getting ventricular tachycardia in atrial fibrillation?
HOWEVER, in atrial fibrillation, there are MANY ripples (i.e. waves of depolarization) hitting the sand castle (AV node), constantly, and so the AV node is constantly being depolarized. Each time the AV node is depolarized enough to launch an action potential, the His Purkinje system (and thus the ventricle) will fire.
Every time a wave of depolarization hits the AV node, will it cause ventricular depolarization? Why or why not?
1) The AV nodal depolarization must reach conduction (action potential) threshold
2) The AV node must NOT be in an absolute refractory period, and must be able to overcome the relative refractory period
What has a lower resting membrane potential – nodal or non-nodal tissue? What is the basis for this?
Non-nodal tissue has a special K+ channel, called IK1. Thus, because a larger proportion of the ion channels open at rest are K+ channels in non-nodal tissue, its resting membrane potential will be much closer to the equilibrium potential of K+.
What ion is primarily responsible for conduction through non-nodal tissue?
What ion is primarily responsible for conduction through the AV node? Why?
In order to activate Na+ channels generally in the heart, you must REMOVE INACTIVATION from them (double-negative, I’m sorry). In order to remove inactivation, you must have a more negative membrane potential. This is ONLY possible in non-nodal tissue, because of the presence of the special K+ channel, called IK1.
In other words, nodal tissues HAS Na+ channels (oddly enough), but it does NOT use them, because the membrane potential does NOT become negative enough to remove inactivation of the Na+ channels.
Ca++ channels do not have this sort of regulation, and thus will be active in nodal tissue.
What is goal of rate control in the context of atrial fibrillation?
What is the basis for rate control in atrial fibrillation?
What major antiarrhythmic classes are used for rate control in atrial fibrillation? Why does this make sense?
We continue with our previous analogy, where every ripple (atrial depolarization) in our pond that reaches the sand castle (AV node) → AV nodal depolarization → Purkinje depolarization → ventricular depolarization.
A calcium channel blocker makes it HARDER to depolarize the AV node (recall that Ca++, not Na+, is required for AV nodal depolarization), sort of like erecting a small barrier in front of our sand castle, so that only larger ripples (waves of depolarization) can actually reach said sand castle.
Wait!
I strongly recommend that you attempt to answer the final questions by yourself first, before looking at the answers. Remember, the USMLE Step 1 exam will test your ability to make connections on the spot. The more practice you have, the higher your score! Then, when you think you might know the answer (or are completely stumped), look at the answers below!
Ready to apply your USMLE Step 1 knowledge?
What is more dangerous – atrial fibrillation or ventricular fibrillation? Why does this make sense?
However, in ventricular fibrillation, it is your VENTRICLE (not your atrium) that is experiencing asynchronous, partial depolarizations (often referred to as “quivering,” owing to how this would appear grossly if you were to look at the heart during fibrillation).
What is the mechanism of ventricular tachycardia in a-fib? Why would a β-blocker or Ca++ channel blocker help?
Each time the atrial depolarizations cause an action potential in the AV node, there will be conduction through the His Purkinje system/ventricles. However, because this AV nodal depolarization is dependent on Ca++, slowing Ca++ influx (accomplished by Ca++ channel/β blockers) → more difficult to get AV node depolarization → fewer atrial depolarizations conducted through to ventricle → lower heart rate (# of ventricular contractions/min)
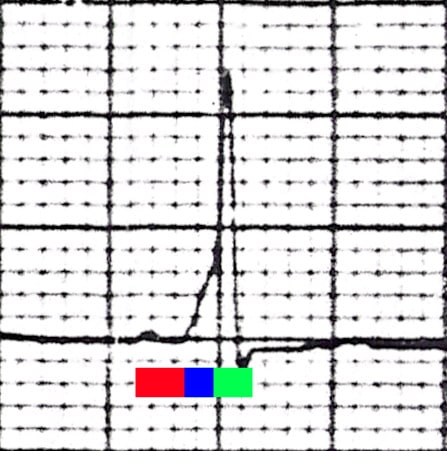
What would be the EKG findings in WPW? Why does this make sense?
QRS wide – some ventricular myocyte-to-myocyte depolarization (i.e. not all of ventricle depolarized by His Purkinje system)
Delta wave – slurred, early upstroke of the QRS due to that part of the ventricle being depolarized early, prior to the rest of the ventricle being depolarized by the His Purkinje system
The red bar represents the PR interval of 0.1 seconds (100 miliseconds). The blue bar represents the slurred upstroke in the QRS complex that is found in WPW syndrome, known as the delta wave. The combination of the blue bar and the green bar make up the QRS complex, which is prolonged (160 miliseconds).
β blockers primarily affect which major EKG interval? How do they affect this interval and why?
NOTE: Ca++ channel blockers will also prolong the PR interval.
What should you do next?
- Turn the narrative, “Pathogenesis to Presentation” questions into Anki cards by copy/pasting the question/answer into the “Front” and “Back” fields in Anki. Do the same for the fundamental facts that you were unfamiliar with, to maximize your chances of USMLE Step 1 success! Remember: the USMLE is a test of understanding, so the better you can understand these questions, the better your score!
- Add reverse cards when appropriate to your Anki cards
- Re-word the questions/explanations as desired, and BOLD the important text to make it easier to review in the future
- Learn something new? Something unclear? Comment below!
- If you liked this post, please consider sharing it on Facebook/Twitter! I judge the utility of these posts by the number of comments / shares they receive, so if you’d like more, or would like a particular topic addressed, please let us know!
Photos by: Tom Lück, Kalumet, Ksheka.







Here’s a better Anki card I think since I didn’t understand the one offered above:
Front:
Na⁺ vs. Ca²⁺ – Use repolarization voltages to explain which is primarily responsible for conduction through the AV node. Why does this make sense?
Back:
Ca²⁺
Summary:
AV node: Ca²⁺ channels conduct → recover at –50 mV
Na⁺ channels need –90 mV
Detailed:
Na⁺ channels require deep repolarization (≈ –90 mV) to recover from inactivation → this only happens in non-nodal tissue with IK1
AV node lacks IK1 → resting Vm ≈ –60 mV
Ca²⁺ channels recover at –50 to –60 mV → remain functional
→ AV node uses Ca²⁺ influx for conduction
Awesome – thanks so much!
Hi,
I have been using your strategy with Anki Cards and it has been working great. I have had some trouble with ANS drugs and I thought I read somewhere on here (though I cannot find it now) that we could get access to a deck of your ANS drug cards? Thanks for all of your help!
Hey Joe!
Thank you so much for your message and positive feedback. Here is the link to the article/free ANS pharm cards:
http://www.yousmle.com/how-to-master-pharmacology-for-the-usmle-step-1-over-a-glass-of-wine/
Best of luck! I look forward to hearing more about what you think about the ANS cards.
Take care,
Alec