Are you applying to residencies and worried about pathology program signals? How do pathology residencies use signals? Do you really need to signal programs in pathology? Will not signaling affect your pathology residency application?
Look below to find the most important data from the most recent ERAS Program Director survey to learn more!
Table of Contents
What is Preference Signaling?
First, let’s describe more about preference signaling and why it’s used. Our guide to preference signaling delves deeper into the specifics and intricacies of preference signaling. In the guide, we have evaluated preference signaling on several parameters. Here is a brief summary for you. Preference signaling serves as a tool for applicants to clearly express their interest in a specific number of residency programs. It also facilitates direct communication with the chosen programs.
By signaling their interest, applicants highlight their authentic preference for the particular program. This helps program directors know which applicants are genuinely interested and thus should get invited to interview. Preference Signaling can thus come to your rescue as well as highlight your application to the program director.
While signaling is still being trialed with a limited number of specialties and programs participating, more are expected to join in 2024.
How Many Signals Are Available in Pathology?
Pathology did not participate in the trial of the 13 programs participating in preference signaling in 2023, but we can see the # of signals of participating specialties below. Check out our Guide to Preference Signaling to see the full list of programs and signals available in 2024.
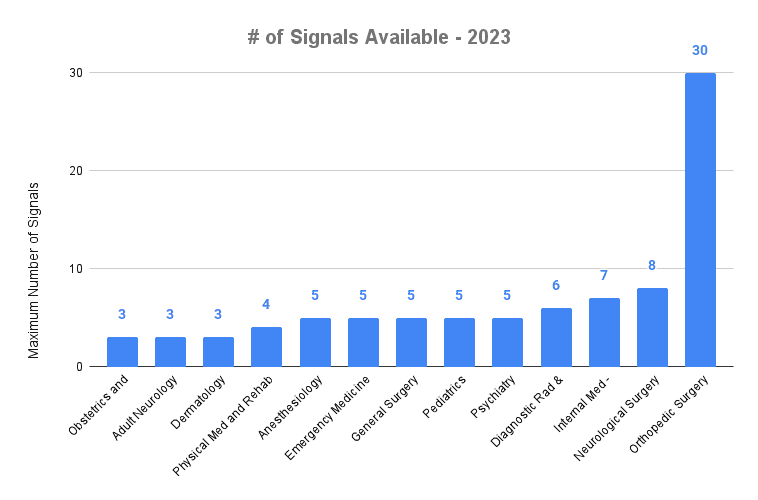
# of Signals Available – 2023
Why do some residency programs have more signals than others? The answer isn’t clear, but the program with the most signals, orthopedic surgery, is historically known to require a large number of applications to increase the chances of matching. Other specialties like anesthesiology, dermatology, and diagnostic radiology are seeing big increases in signals available in 2024, so the system is still a work in progress.
The table below shows the participating specialties and signals for the 2024 match cycle.
| Specialty | Number of Program Signals |
|---|---|
| Anesthesiology | 5 (gold), 10 (silver) |
| Child Neurology & Neurodevelopmental Disabilities | 3 |
| Dermatology | 3 (gold), 25 (silver) |
| Diagnostic Radiology and Interventional Radiology | 6 (gold), 6 (silver) |
| Emergency Medicine | 7 |
| Family Medicine | 5 |
| General Surgery | 5 |
| Internal Medicine | 7 |
| Internal Medicine & Psychiatry | 2 |
| Neurological Surgery | 25 |
| Neurology | 3 |
| Obstetrics and Gynecology | 3 (gold), 15 (silver) |
| Orthopedic Surgery | 30 |
| Otolaryngology | 25 |
| Pathology | 5 |
| Pediatrics | 5 |
| Physical Medicine and Rehabilitation | 5 |
| Public Health and General Preventive Medicine | 3 |
| Psychiatry | 5 |
| Thoracic Surgery | 3 |
How Will Pathology Programs Use Signals?
Signaling was a big change to the application process in 2023, but did signals change how PDs chose which applicants to interview?
How PDs decide who to interview and how they weigh different experiences, attributes, and academic metrics is largely a mystery and different in each program. Standing out can be difficult with so many applications, so can signals help you stand out?
While we don’t yet have data for pathology, we can look at other specialties to know what can be expected. In the 2022-2023 Supplemental ERAS Program Director Survey, program directors were asked about the importance of signals at each stage of the application process. You can see how PDs answered below along with the importance of each stage.
| How important were program signals at each of the following stages of the application review process? | n | Did Not Use % (n) | Used % (n) | Not Important % (n) | Somewhat Important % (n) | Important % (n) | Very Important % (n) | Important or Very Important % (n) |
|---|---|---|---|---|---|---|---|---|
| As a screening tool, before a more thorough application review | 824 | 12% (102) | 88% (722) | 9% (63) | 21% (152) | 25% (183) | 45% (324) | 70% (507) |
| Sending interview invitations to every applicant who signaled my program | 817 | 39% (318) | 61% (499) | 43% (214) | 29% (147) | 16% (82) | 11% (56) | 28% (138) |
| Including in a composite filter to conduct holistic review | 814 | 22% (176) | 78% (638) | 13% (81) | 26% (163) | 34% (214) | 28% (180) | 62% (394) |
| As part of a holistic process to help decide who to interview | 819 | 9% (71) | 91% (748) | 6% (46) | 27% (199) | 34% (257) | 33% (246) | 67% (503) |
| As a tie breaker when deciding who to interview | 816 | 14% (116) | 86% (700) | 10% (73) | 25% (175) | 33% (228) | 32% (224) | 65% (452) |
| During the interview to learn more about why an applicant signaled my program | 815 | 36% (292) | 64% (523) | 25% (130) | 33% (173) | 25% (132) | 17% (88) | 42% (220) |
| Plan to use during ROL discussion | 814 | 37% (299) | 63% (515) | 28% (144) | 35% (182) | 24% (124) | 13% (65) | 37% (189) |
| Other | 241 | 73% (175) | 27% (66) | 36% (24) | 33% (22) | 15% (10) | 15% (10) | 30% (20) |
Signal Importance as a Screening Tool
Before selection for interview invites begins, programs must first screen applications to decide who would (or would not) be a good candidate for holistic review. Anesthesiology was at the top of specialties surveyed with 88% of PDs finding signaling to be important or very important as a screening tool. Neurological surgery, emergency medicine, and general surgery were below the average with only 30%, 46%, and 57% respectively.
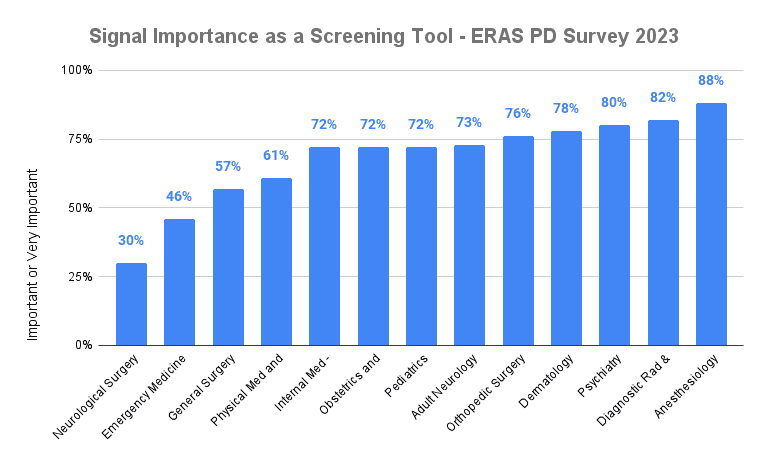
Signal Importance as a Screening Tool – ERAS PD Survey 2023
Signal Importance as Part of Holistic Review
While screening is the first hurdle for most applications, holistic review is where your experiences and application as a whole can be properly evaluated. While all specialties considered signals important as a part of holistic review, 80% of diagnostic radiology and interventional radiology PDs thought signals were important or very important, but emergency medicine, neurological surgery, general surgery, and adult neurology were on the lower end with 51%, 54%, 57%, and 58% respectively.
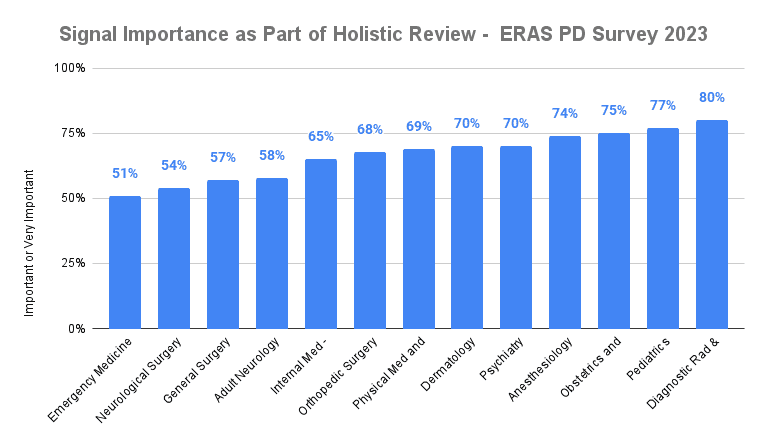
Signal Importance as Part of Holistic Review – ERAS PD Survey 2023
Signal Importance as a Tie Breaker in Pathology
When deciding between two equal applicants to interview, all specialties found signals to be important as a tie breaker. Diagnostic radiology and interventional radiology again is at the top of all residencies with 73% of PDs finding signals as important or very important as a tie breaker. Emergency medicine and dermatology were the lowest with 55% and 59%.
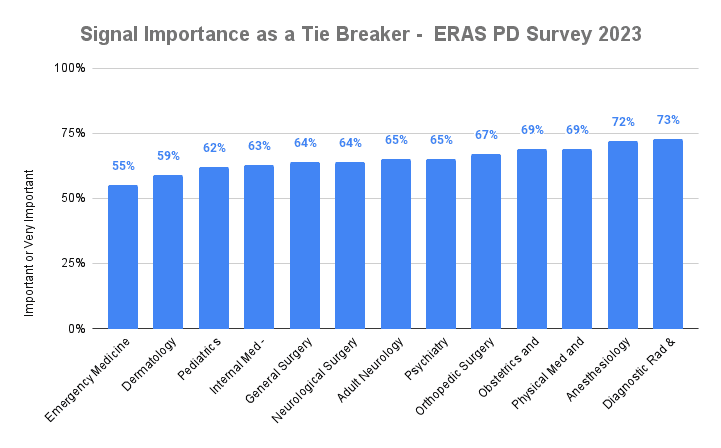
Signal Importance as a Tie Breaker – ERAS PD Survey 2023
Do I Need to Signal Pathology Programs to Get an Interview?
As more specialties are adding the supplemental ERAS application, signals will become an important tool for applicants. Signals are meant to highlight an application and show interest in a program. So will this change how programs view applications without signals? Do residency applications without signals get treated differently?
The answer is, it depends.
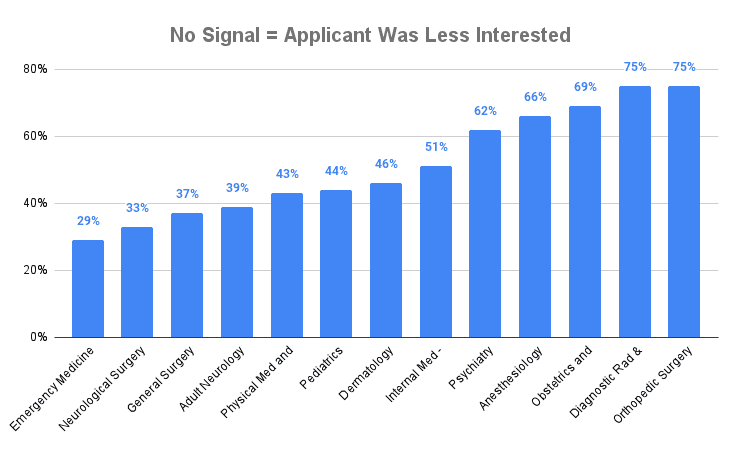
Looking at how PDs viewed applications, a blank signal value may be interpreted negatively. This could be especially true for orthopedic surgery and diagnostic and interventional radiology with 75% of PDs interpreting a blank signal as meaning the applicant was less interested in the program. Emergency medicine, neurological surgery, and general surgery ranked lowest with 29%, 33%, and 37% respectively.
Is lower interest a bad thing? Not inherently, but as we saw before with tie breakers, it could make the difference between getting an interview or not.
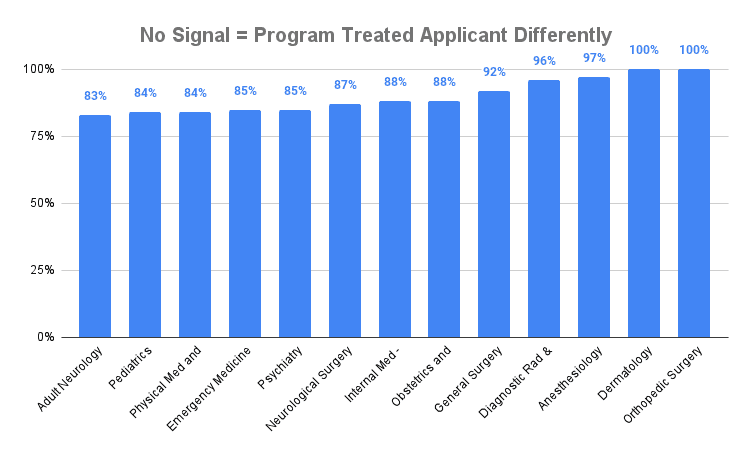
PDs were also asked if signaled applicants were treated differently than no signal. We can assume this means that at some point in the application review process, signals were considered.
Orthopedic surgery and dermatology ranked the highest with 100% of PDs treating no-signal applicants differently than those who signaled. Specialties that responded on the lower end are generally viewed to be less competitive with pediatrics, physical med and rehab, and emergency medicine responding at 84% to 85%.
You can see the all results for all specialties in the table below.
| All Specialties: PD interpretation of no signal | Applicant was less interested in my program | Applicant was willing to go anywhere | Applicant was afraid or unwilling to provide a response | Did not draw any conclusions | Treated the same as applicants who signaled my program | Other |
|---|---|---|---|---|---|---|
| Adult Neurology | 39% | 17% | 6% | 53% | 17% | 0% |
| Anesthesiology | 66% | 10% | 5% | 32% | 3% | 2% |
| Dermatology | 46% | 21% | 14% | 29% | 0% | 14% |
| Diagnostic Rad & Interventional Rad | 75% | 14% | 8% | 24% | 4% | 0% |
| Emergency Medicine | 29% | 13% | 3% | 62% | 15% | 5% |
| General Surgery | 37% | 11% | 5% | 56% | 8% | 5% |
| Internal Med - Categorical | 51% | 23% | 14% | 33% | 12% | 5% |
| Neurological Surgery | 33% | 27% | 13% | 47% | 13% | 0% |
| Obstetrics and Gynecology | 69% | 17% | 8% | 25% | 12% | 6% |
| Orthopedic Surgery | 75% | 8% | 10% | 18% | 0% | 5% |
| Pediatrics | 44% | 13% | 20% | 48% | 16% | 3% |
| Physical Med and Rehab | 43% | 19% | 16% | 43% | 16% | 5% |
| Psychiatry | 62% | 14% | 9% | 30% | 15% | 1% |
What are the Advantages of Program Signaling?
Pros: Preference signaling acts as a bridge. It aids applicants and program directors alike in finding the right match. For applicants, it’s an avenue to express genuine interest leading to increased interview invitations. Program directors get a streamlined selection process. Signals help identify candidates aligned with their program’s values.
Cons: Blank signals carry a risk of getting misinterpreted. A program director may draw false assumptions about an applicant who leaves blank signals. There’s also the concern of unfair advantages, where applicants who strategically signal might gain an upper hand.
Balancing transparency with integrity is vital. Preference signaling is relatively new to medical residency applications. It has only recently evolved from a nascent stage. Striking balance is essential to ensure a fair and authentic selection process.
Pathology Signaling Strategies
- Use all the signals available to you for your specialty.
- While it’s been advised to not signal your home program, check with the program director first to confirm this until programs are adapted to the system
- Note that each applicant should take an individualized approach to sending signals. Consider factors such as application strength, overall competitiveness, career goals, and personal circumstances relative to the program’s mission before you choose where to signal.
- Discuss with mentors and faculty to work out the programs where to send signals.
- Consider the geographic preference
- Sending signals may or may not result in a higher number of interview invitations. There are no guarantees.
Conclusion
Signaling is just one of the changes being implemented to help level the playing field for future applicants. While signals may play a larger role, it isn’t likely to increase matching chances more than having a well-rounded application. This includes avoiding any failed Step tests and getting the highest Step 2 CK score possible.
If you are feeling overwhelmed, you aren’t alone. We offer free consultations for students to help identify what is them back and how best to break through to help match into their dream residency. If you need to talk, book a consultation today and receive free lectures and Anki cards from the Yousmle Library on the topics students struggle with most!