While many medical students diligently try to understand the mechanisms of disease in order to succeed on the USMLE Step 1, one of the hardest topics to do so is anemias. Specifically, connecting the mechanism of anemia with anything else – be it the MCV (mean corpuscular volume), the TIBC, or even the transferrin saturation levels, is a daunting challenge, one that has tripped up many a medical student. Here, by walking through the mechanism of anemia, we will be able to learn these topics to the depth I used to score a 270 on the USMLE Step 1. In addition to being able to connect the mechanism of anemia to MCV, by the end, you will be able to answer the following questions:
- Anemia of chronic disease – use mechanism of disease to explain iron panel results (TIBC, ferritin, transferrin sat, serum iron)
- Iron-deficiency anemia – use mechanism of disease to explain iron panel results (TIBC, ferritin, transferrin sat, serum iron)
- Sideroblastic anemia – using the mechanism, explain what the iron panel results would be?
Ready to start?
What is the major function of RBCs?
What ion allows for O2 to bind to hemoglobin? What is the oxidation state?
What molecule is this iron a part of?
What is methemoglobin? What is the problem with having too much methemoglobin?
What is MCV (mean corpuscular volume)?
What is the difference between hemoglobin and heme? Which actually binds O2?
Hemoglobin is a protein composed of 4 globin protein subunits, each containing 1 heme molecule.
What is anemia?
What is a microcytic anemia? A normocytic anemia?
In a normocytic anemia, each RBC is “normal” in size.
So what would a macrocytic anemia be?
Microcytic anemias – what are the MCV (mean corpuscular volume) values associated with it? Generally speaking, what will cause a microcytic anemia?
Normocytic anemias – what are the MCV values associated with it? Generally speaking, what will cause a normocytic anemia?
Macrocytic anemias – what are the MCV values associated with it? Generally speaking, what will cause a macrocytic anemia?
Anything that diminishes DNA synthesis
The way to think about it is that during RBC development, as the RBC “balloons” are filling with the hemoglobin protein, if DNA replication is too slow because there are too few nucleotides, then the RBCs will become “overfilled”
Thalassemias - generally speaking, what is the defect?
We will discuss elsewhere the thalassemias, and how their underlying defect explains what you see on hemoglobin electrophoresis
Thalassemias - using the underlying defect, explain what kind of anemia it would cause (microcytic, normocytic, macrocytic). Why does this make sense?
In other words, the RBC “balloon” is less full of hemoglobin, so the volume of each RBC will be less
What kind of anemia (microcytic, macrocytic, normocytic) would iron-deficiency anemia lead to? Why?
Hydroxyurea - what is the mechanism of action?
What kind of anemia (microcytic, macrocytic, normocytic) would hydroxyurea lead to? Why?
What kind of anemia (microcytic, macrocytic, normocytic) would B12-deficiency anemia lead to? Why?
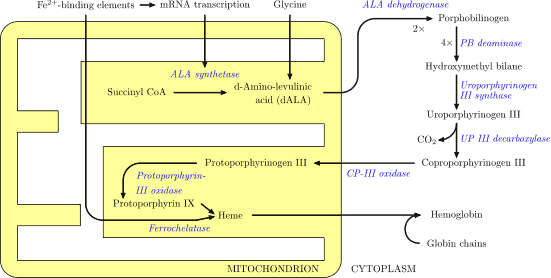
Don’t worry – you won’t have to memorize all of this!
I know this is a lot of information
What are the components of an iron panel? (4)
Serum iron
TIBC (total iron binding capacity)
Transferrin saturation
What is the function of ferritin? What do we use it for diagnostically?
Ferritin levels in the blood correlate with ferritin levels in your body (i.e. the total amount of stored iron)
What is the function of transferrin? What do we use transferrin saturation for diagnostically?
Transferrin saturation levels are higher when iron levels are higher
What is the difference between “transferrin” and “transferrin saturation”?
Transferrin saturation = % of transferring bound to iron
(analogous to hemoglobin saturation, which is the % of total hemoglobin that is bound to O2)
What will transferrin saturation generally correlate with?
Ferroportin – what is its function in the body? (2)
What is hepcidin? What does it lead to?
CAUSES FERROPORTIN TO BE INTERNALIZED/DEGRADED
For clarity, I will include previous definitions for reference:
Transferrin = molecule that carries iron in the blood
Transferrin saturation = % of transferring bound to iron
(analogous to hemoglobin saturation, which is the % of total hemoglobin that is bound to O2)
Ferroportin – Transport of iron into the blood from: intestinal epithelial cells, and bone marrow macrophages
If I degrade ferroportin, what will be the effects on iron absorption in my body? Why?
Ferroportin allows for iron absorption into my blood stream, so if I degrade the protein → less iron absorption
If I degrade ferroportin, what will be the effects on release of iron stored in bone marrow macrophages? Why?
Ferroportin allows for bone marrow macrophage iron release, thus hepcidin → ↓ iron release from bone marrow macrophages
What causes release of hepcidin?
What determines TIBC (total iron binding capacity)? What is the relationship between TIBC and ferritin (positive correlation, negative correlation, no correlation)?
There is a NEGATIVE correlation between TIBC and ferritin. The way you can think about this is high TIBC indicates your body is “looking for iron.” In other words, if iron stores are low, it makes sense that your TIBC/transferrin would be high, since in cases of low stores of iron, your body would be trying to “find” iron.
Hepcidin – Why would it make sense that a molecule like this would exist? Why does this relationship between TIBC/transferrin and ferritin make sense?
Anemia of chronic disease – what is the mechanism?
Chronic inflammation → chronic IL-6 production → chronic hepcidin production → iron absorption ↓, release of iron from stores ↓
→ insufficient iron for adequate heme production → hemoglobin ↓
Sideroblastic anemia – what is the mechanism of disease?
Wait!
I strongly recommend that you attempt to answer the final questions by yourself first, before looking at the answers. Remember, the USMLE Step 1 exam will test your ability to make connections on the spot. The more practice you have, the higher your score! Then, when you think you might know the answer (or are completely stumped), look at the answers below!
Ready for the answers?
Iron-deficiency anemia – use mechanism of disease to explain iron panel results (TIBC, ferritin, transferrin sat, serum iron)
Anemia of chronic disease – use mechanism of disease to explain iron panel results (TIBC, ferritin, transferrin sat, serum iron)
Sideroblastic anemia – using the mechanism, explain what the iron panel results would be?
However, there are no issues with iron absorption. Thus, serum iron levels / transferrin saturation would be ↑, as would ferritin. Ferritin ↑ → TIBC ↓
What should you do next?
- Turn the narrative, “Pathogenesis to Presentation” questions into Anki cards by copy/pasting the question/answer into the “Front” and “Back” fields in Anki. Do the same for the fundamental facts that you were unfamiliar with, to maximize your chances of USMLE Step 1 success! Remember: the USMLE is a test of understanding, so the better you can understand these questions, the better your score!
- Add reverse cards when appropriate to your Anki cards
- Re-word the questions/explanations as desired, and BOLD the important text to make it easier to review in the future
- Learn something new? Something unclear? Comment below!
- If you liked this post, please consider sharing it on Facebook/Twitter! I judge the utility of these posts by the number of comments / shares they receive, so if you’d like more, or would like a particular topic addressed, please let us know!
Photo from Wikimedia Commons.







What’s “Pathogenesis to Presentation”? Where do I find it? …or is it your anemia questions here?
Great question – I address how to learn in a pathogenesis to presentation manner here: https://www.yousmle.com/nail-fundamentals-usmle-step-1-nbme-practice-exams/
Hi
I just wanted to let you know that I really enjoyed reading your questions.
Awesome – thanks for the feedback!!
Goodness finally someone explains it.
Thanks for the positive feedback John! Be sure to check out the other articles, and let me know how better I can help!!